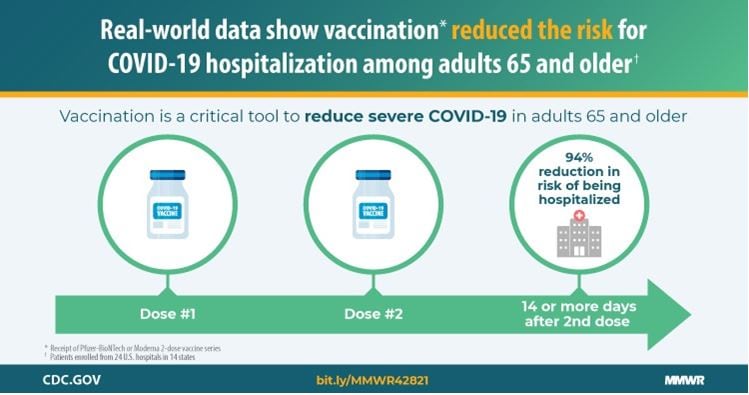
Getting vaccinated prevents severe illness, hospitalizations and death. People 65 and older who received both doses of either Pfizer or Moderna vaccines showed a 94% reduced risk of COVID-19 related hospitalization. Unvaccinated people should get vaccinated and continue masking until they are fully vaccinated. With the Delta variant, this is more urgent than ever. CDC has updated guidance for fully vaccinated people based on new evidence on the Delta variant.
Disparities in COVID-19 Vaccination Coverage Among Staff in Long Term Care Facilities
Achieving high vaccination coverage in long-term care facilities is critical to preventing additional outbreaks of COVID-19. Vaccination coverage was highest among physicians (75.1%) and lowest among aides (45.6%). Vaccination rates among aides was lower in facilities located in zip code areas with higher levels of social vulnerability. Morbidity and Mortality Weekly Report, July 30, 2021.
When You’ve Been Fully Vaccinated
If you are fully vaccinated, you can participate in many of the activities that you did before the pandemic.

- UPDATED What You Can Do Once You’re Fully Vaccinated
- Choosing Safer Activities
- Have You Been Fully Vaccinated?
- Key things to know about COVID-19 vaccines
- Find a vaccine
What Older Adults Need to Know about COVID-19 Vaccines
The risk of severe illness from COVID-19 increases with age. This is why CDC recommends that adults 65 years and older receive COVID-19 vaccines. Getting a COVID-19 vaccine is an important step to help prevent getting sick from COVID-19.

- Tips for how to get a COVID-19 vaccine
- Search vaccine providers near youexternal icon
- Vaccine considerations for people with allergies
- Vaccine considerations for people with underlying medical conditions
- Recommendations for visiting long-term care facilities
- Centers for Medicare and Medicaid Services guidance for visitationsexternal icon
Guidance for Older Adults at Higher Risk

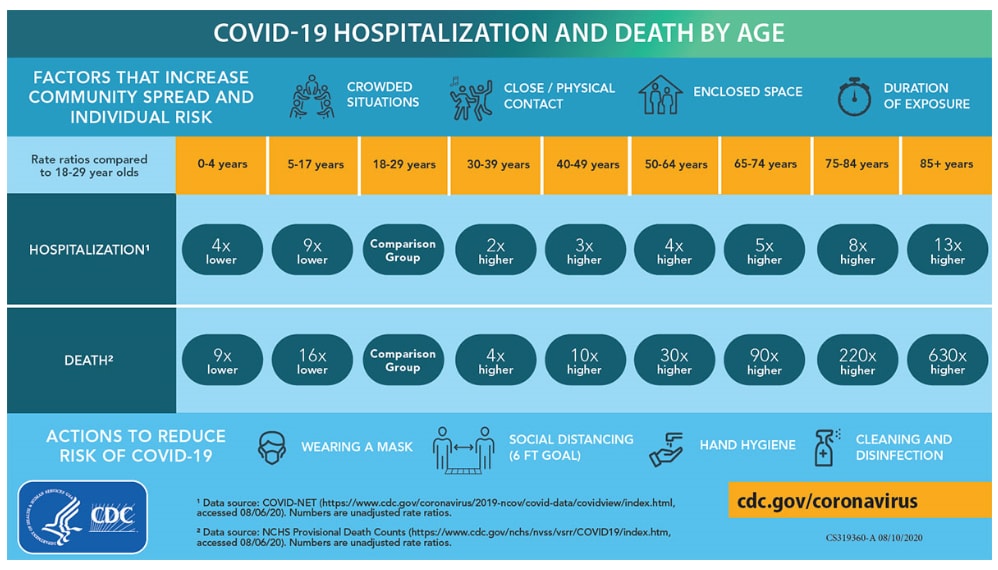
The more closely you interact with others and the longer that interaction lasts, the higher the risk of COVID-19 spreading.
- Guidance for Older Adults
- Daily Activities and Going Out
- People at Increased Risk
- Racial and Ethnic Minority Groups
- Symptoms of Coronavirus
COVID-19 and Mental Health: How Are You Feeling Right Now?
During the COVID-19 pandemic, we are often asked, “How are you feeling?” but this has been a difficult time lately, and emotions can be complex. Whatever you’re feeling right now, starting a conversation with friends, neighbors, and loved ones about your concerns can relieve stress and promote resilience. Learn how to start the conversation, find tools, resources, and inspiration all provided by the CDC Foundation, HowRightNow.orgexternal icon

COVID-19 Guidance for Adult Day Service Center Participants and Their Caregivers
Adult Day Service Centers (ADSCs), also known as adult day services or adult day care, provide social or health services to adults 65 and older living in communities and to adults of any age living with disability. CDC has developed guidance for participants and their caregivers to help reduce the spread of COVID-19 at ADSC facilities and at home.
- UPDATED Summary of Recent Changes
- What you can do to protect yourself and others
- What to do if you are sick or have been exposed to COVID-19
- What to do if you are worried, stressed, or sad
- Additional resources
COVID-19 Key Points for Adult Day Service Center Administrators and Staff
Adult Day Service Centers (ADSCs) administrators and staff can help protect themselves and program participants (that is, adults attending ADSCs) from COVID-19 by promoting and engaging in preventive behaviors that reduce spread and maintain healthy operations and environments at ADSC facilities.

- UPDATED Summary of Recent Changes
- Promoting Vaccination
- Wearing Masks and Physical Distancing
- Improving Ventilation
- Hand Hygiene and Respiratory Etiquette
- Encouraging Everyone to Stay Home When Sick
- Cleaning and Disinfecting
- Mental Health Resources, Other Resources
COVID-19 Vaccines in Older Adults Reduce Deaths, Hospital Visits, and Number of Cases
As of May 1, 2021, 82% of adults aged 65 and older had received at least one dose of a COVID-19 vaccine. The number of COVID-19 cases, emergency department visits, hospital admissions, and deaths declined more in older adults, who had higher vaccination coverage, than in younger adults, who had lower coverage. Morbidity and Mortality Weekly Report, June 8, 2021.
COVID-19 Vaccines Significantly Reduce Risk for Hospitalization in Older Adults
Adults 65 and older who received both doses of either Pfizer-BioNTech or Moderna COVID-19 vaccines showed a 94% reduced risk of COVID-19-related hospitalization. An evaluation was conducted at 24 hospitals in 14 states under real-world conditions, January – March 2021. Morbidity and Mortality Weekly Report, April 28, 2021.
COVID-19 Cases Among Nursing Home Residents and Staff Mirror Community Spread
Rates of COVID-19 among nursing home residents and staff members increased during June and July 2020 and again in November. Trends in reported cases of COVID-19 cases among nursing home residents and staff members were similar to trends in incidence of COVID-19 in surrounding communities. Morbidity and Mortality Weekly Report, January 9, 2021.

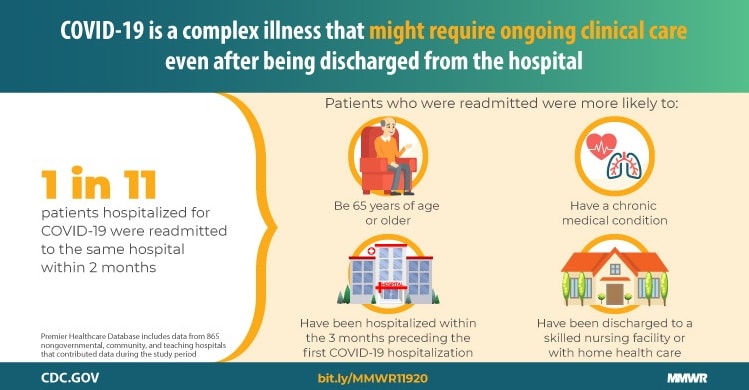
1 in 11 Patients Who Were Hospitalized for COVID-19 Were Readmitted
An analysis of more than 106,000 patients who survived COVID-19 showed that 9% (9,504) were readmitted to the same hospital within 2 months of discharge, according to the Morbidity and Mortality Weekly Report, Nov. 9, 2020. The odds of hospital readmission increased with age and the presence of 5 chronic health conditions: COPD, heart failure, diabetes, chronic kidney disease, and obesity.
Older Adults Die More Frequently from COVID-19
An analysis of more than 114,000 COVID-19 associated deaths during May – August 2020, found that 78% of the people who died were aged 65 and older, and 53% were male; 51% were White, 24% were Hispanic, and nearly 19% were Black. COVID-19 remains a major public health concern regardless of age or race and ethnicity. Morbidity and Mortality Weekly Report, Oct. 16, 2020.
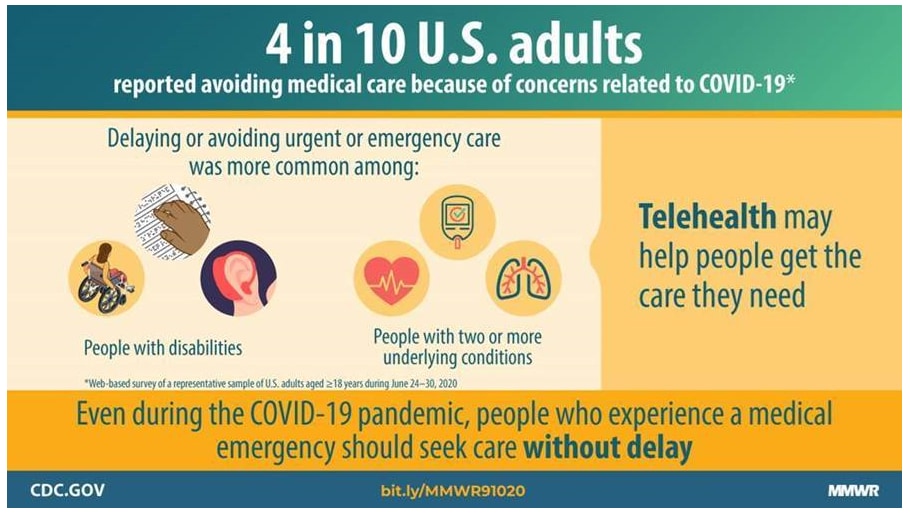
Adults Delay Medical Care Due to COVID-19 Concerns
An estimated 41% of U.S. adults reported avoiding medical care because of concerns about COVID-19, including 12% who avoided urgent or emergency care, and 32% who avoided routine care. Even during the COVID-19 pandemic, people who experience a medical emergency should seek medical care without delay. Morbidity and Mortality Weekly Report, Sept. 11, 2020.
Tribal Communities
American Indian/Alaska Native communities with multi-generational households or those in rural or tribal areas may experience unique challenges with social distancing, access to grocery stores, water, and local and tribal health services. Here are several steps individuals can take to keep your home and family safe.
- Plan, Prepare, and Respond
- Social Distancing for Tribal Communities with Local COVID-19 Transmission, including Tips for Multi-generational Households.
- Care for Breastfeeding Women (Updated)
Develop a Care Plan
Developing a care plan is vital during this crucial time in our country. A care plan is a form that summarizes a person’s health conditions and current treatments.
Disability Groups and Risk
Some people with disabilities might be at a higher risk of infection or severe illness from COVID-19. Find out who may be at risk and how to protect yourself.
Considerations for Memory Care Units in Long-term Care Facilities
At least half of older adults living in long-term care facilities have cognitive impairment such as Alzheimer’s disease or a related dementia. The first step in caring for people living with dementia in any setting is to understand that changes in behavior (e.g., increased agitation, confusion, sudden sadness) or worsening symptoms of dementia should be evaluated because they can be an indication of worsening stress and anxiety as well as COVID-19 or other infections.
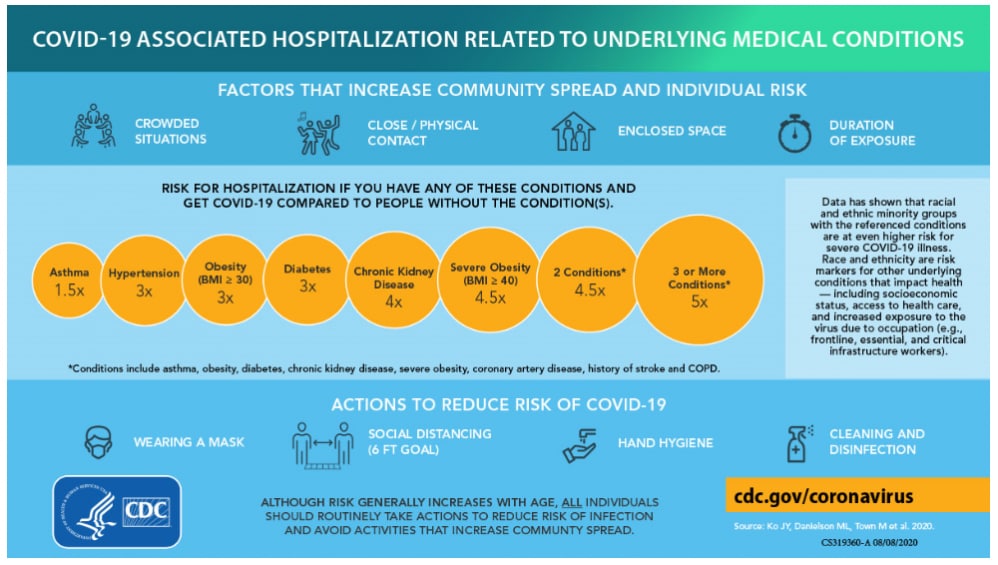
COVID-19 Risk of Hospitalization If You Have These Health Conditions
Chronic health conditions such as diabetes increases your risk of being hospitalized from COVID-19. For more information, see COVID-19 Associated Hospitalization Related to Underlying Medical Conditions.
Key Strategies for Long-term Care Facilities
COVID-19 cases have been reported in all 50 states, the District of Columbia, and multiple U.S. territories; many having wide-spread community transmission. Given the high risk of spread once COVID-19 enters a long-term care facility (LTCF), facilities must act immediately to protect residents, families, and staff from serious illness, complications, and death.
- Key Strategies to Prepare and Respond to COVID-19 in Long Term Care Facilities
- Preparedness Checklist for Facilities pdf icon[PDF – 1MB]
- Testing for COVID-19 in Nursing Homes
- Caring for Patients with Confirmed or Suspected COVID-19
Communication Resources
Videos in American Sign Language
COVID-19 guidance is available in American Sign Language on the CDC YouTube Channel. 20 videos are currently posted.
COVID-19 Hospitalization and Death by Age
As you get older, your risk of being hospitalized or dying from COVID-19 increases.